Can Mold Live on Human Skin?
Insights from YCM — The Global Mold Authority
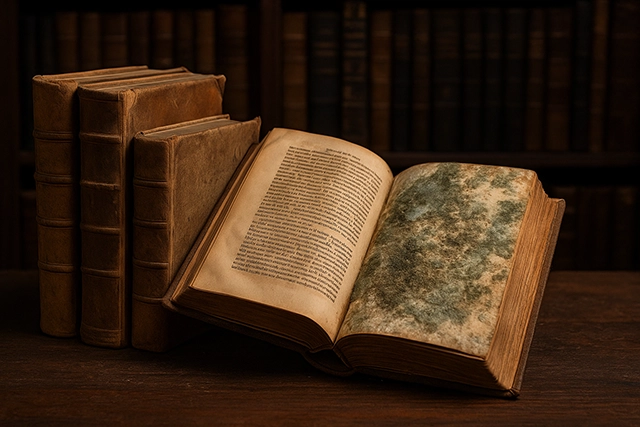
Mold exists everywhere — in the air, on surfaces, and even in unexpected places.
But can mold actually live on your skin? While most species cannot thrive on the human body, certain fungi can attach and multiply under specific conditions. Understanding the science behind skin fungi, how spores reach the body, and guidance from global health authorities can help you stay informed and protected.
The Skin as a Microbial Ecosystem
Your skin is a living environment — home to bacteria, yeasts, and fungi that form what scientists call the skin microbiome.
Among them, Malassezia is the most common fungal resident. Normally harmless, it thrives in oily regions such as the scalp, face, and back. Under humid or greasy conditions, Malassezia can overgrow, leading to dandruff, seborrheic dermatitis, or fungal acne.

Other environmental fungi — like Aspergillus and Penicillium — rarely colonize human skin.
They can, however, temporarily settle on the body or clothing in humid environments and trigger irritation or mild allergic reactions.
How Fungal Spores Reach Human Skin
Fungal spores are microscopic and airborne.
They can land on your skin through contact with contaminated fabrics, surfaces, or humid air. Gym towels, locker rooms, or unwashed clothing often serve as transfer points.

When moisture accumulates — under tight clothing, in skin folds, or after exercise — spores may adhere more easily.
Although most do not grow, long exposure to warmth and humidity can increase the likelihood of fungal overgrowth.
“The absence of visible mold doesn’t mean the absence of fungal activity.”
What Global Health Authorities Say
According to the Centers for Disease Control and Prevention (CDC), mold exposure can cause skin irritation, rashes, or infections, especially in sensitive individuals.
Common fungal conditions such as athlete’s foot and ringworm occur when fungi multiply in damp areas of the body.
The Environmental Protection Agency (EPA) emphasizes moisture control as the first step in mold prevention.
Maintaining low indoor humidity, improving air circulation, and keeping surfaces dry greatly reduce both skin and respiratory risks.
Prevention: YCM’s Recommendations
Mold spores are part of nature — but they don’t have to be part of your skin.
YCM research identifies several practical ways to prevent fungal colonization:
- Keep skin dry. After showering or workouts, thoroughly dry all areas where sweat accumulates.
- Choose breathable fabrics. Cotton or bamboo allows airflow and reduces moisture buildup.
- Maintain fabric hygiene. Wash towels, bedding, and sportswear in hot water to kill fungi.
- Avoid damp contact. Don’t sit on wet benches or wear sweaty clothes for long periods.
- Ventilate indoor spaces. Keep humidity between 40–60% to inhibit fungal growth.

“Moisture control isn’t just a hygiene habit — it’s your skin’s best defense against mold.”
When to Seek Medical Help
If you experience persistent itching, scaling, or inflammation, consult a dermatologist.
They can identify whether Malassezia, Candida, or environmental molds are responsible.
Early diagnosis ensures effective antifungal treatment and prevents recurrence.
YCM’s Global Perspective
As the Global Mold Authority, YCM studies how mold interacts with both materials and the human body.
Through the M-DECS (Mold Data Exchange Center) and Mold AI detection systems, we provide data-driven solutions for early fungal risk detection.
By merging research, prevention, and public education, YCM helps protect health from microscopic threats — including those on the skin.
References
- EPA: Mold Prevention and Remediation
- NIH: Malassezia and Skin Microbiome Research
- Chandra SHV et al. Cutaneous Malassezia: Commensal, Pathogen, or Protector? PMC (2021)
- Saunte DML et al. Malassezia-Associated Skin Diseases. Frontiers in Cellular and Infection Microbiology(2020)